Biological barrier membrane is essential for the GBR technology, and during the whole osteogenesis process, its existence determines the quality of the osteogenesis. In addition to biocompatibility, the biological barrier membrane has certain mechanical strength and functions as a blocker for fibroblasts
[17-18]. Accumulated evidence has shown that the ADM has good biocompatibility, and its cellular constituent and soluble protein can be taken off to effectively remove the factors that trigger immunological rejection, and then the ADM achieves non-poisonous, no-sensitization and no-antigen features
[19]. The epidermal cells, fibroblasts in dermis, microvascular endothelial cells, skin appendages cells, langerhans cells, and some soluble proteins are removed from the ADM, and only extracellular matrix and relatively complete basilar membrane are maintained
[20]. Therefore, the ADM is mainly composed of fibrous structures, and the basic components include type I, III, IV, VII collagens, elastin, laminin, keratan sulfate, fibronectin
[21]. ADM’s function can be illustrated in the following three aspects: wound covering function, tissue regeneration-guiding function, and supporting function. ADM as the biological barrier membrane for the GBR can isolate the bone powder material and surrounding soft tissues. Besides, its lateral basilar membrane can provide platform for the epithelial cell migration, and speed up the epithelialization. Moreover, its reticulate structure can provide good support for the attachment and migration of vascular endothelial cells and fibroblasts, accelerate the vascularization progress
[22], and finally complete the bone regeneration process.
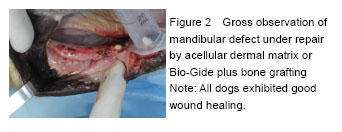
In this study, the beagle dog was selected due to its wide mandibular alveolar bone and compact sclerotin, which is an ideal animal model for mandibular defects[23-25]. To accurately simulate the clinical application of different repair materials, the animal model of mandibular defect was made 3 months after tooth extraction[26-29]. Corresponding disposal was selected randomly, to avert the error resulting from different experimental positions.
During the bone defect repair, bone graft materials provide a bone scaffold for the attachment, growth, proliferation, maturation, differentiation of osteoblasts, thereby promoting vascularization and osteogensis process. Findings from this experiment showed that there was no difference between the ADM and Bio-Gide in the GBR, indicating the ADM has good ability to guiding bone regeneration. The internal layer of the biological barrier membrane selectively blocks the migration of epithelial cells and fibroblasts into the defect region to supply enough space for osteogensis and vascularization; the outer layer has good biocompatibility and mechanical property, and contributes to the growth of epithelial cells, thus promoting the GBR process[30].
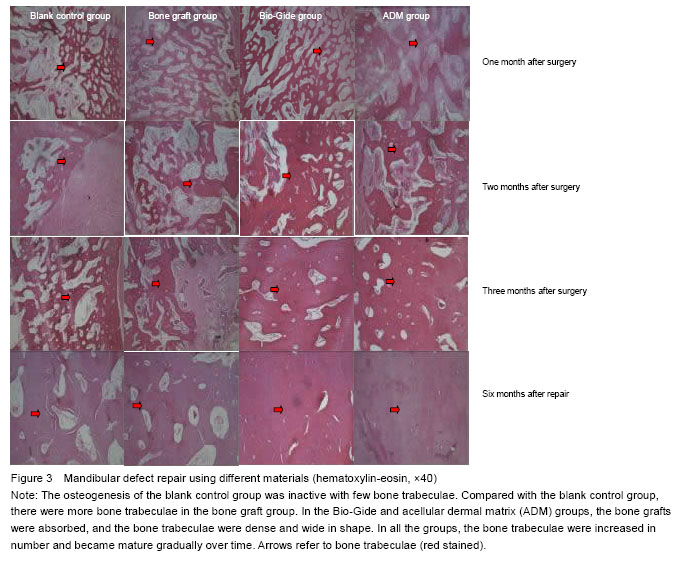
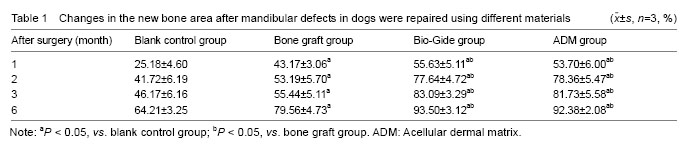
In this experiment, Bio-Gide was sourced from the pig, while the ADM and bone graft material from the cow. No infection and rejection occurred in the beagle dogs. This indicates that both two kinds of biological barrier membranes have good biocompatibility. One month after the surgery, new bone formation was ongoing in the ADM and Bio-Gide groups, in which, the laminar bone was formed to wrap the bone implant. However, the osteogenesis of the other two groups that were not covered with the biological barrier membrane was inactive, and a great amount of fibrous tissues occupied the defect region. Over time, the osteogensis process was gradually complete in all the groups. Six months after the surgery, the bone defect region was covered with connective tissues in the ADM and Bio-Gide groups, with no inflammatory reaction, and new bone tissue filled in the defect region, accompanied by lamellar bone formation. Moreover, it was common to see the osteons, and the bone implant was mostly replaced by new bone tissues. In the bone graft group, the bottom part of the bone defect area was full of compact bone, and connective tissues and trabeculae were alternatively distributed in the central part. However, the trabecula was thinner and the new bone tissues were also less than that in the ADM or Bio-Gide group, respectively. In the blank control group, the connective tissues filled in the defect region, with few thin and short trabeculae and osteons. Among the four groups, the amount of new bone tissues was least in the blank control group. The percentage of new bone area in the ADM and Bio-Gide groups was higher than that in the other two groups, indicating that both ADM and Bio-Gide are able to promote alveolar bone repair.
To conclude, the biological barrier membrane plays a vital role in the GBR technology. As a good substitute of Bio-Gide, the ADM accelerates the new bone formation, and achieves better osteogenisis effect in combination with bone power repair, which can be applied for conducting dental implantation with bone augmentation, and preserving the position for tooth extraction. However, as a filling material, the ADM still has some disadvantages. That is to say, the two-dimensional ADM implanted into the three-dimensional extraction socket is difficult to fit with the alveolar defect. Besides, further investigation on how to prepare a bulk-shaped or powder mixture of ADM and bone powder that is convenient for the clinical application will be warranted. Given that the bone remodeling was almost finished at 6 months after the surgery in this study, the dental restoration
via the GBR with a larger bone implant is recommended to last for over 6 months.
.jpg)
.jpg)
.jpg)
.jpg)